Young Maggie’s
A new model of support for parents and carers of children and young people living with chronic and life-threatening conditions.

|
 |
 |
The Research
Parents and caregivers of children and young people living with chronic and life-limiting conditions
face significant psychosocial challenges1
The Need
Parent difficulties include:
- Fatigue and below-average quality of life2
- Increased risk of mortality after the death of a child or young person3
- Increase risk for mental disorder: acute stress disorder (49–54%); depression and anxiety (15–27%); and stress (25–31%)4
- Lower physical, functional and family well-being scores (parents of palliative care patients) compared with Australian normative data5
- Social isolation5, 6
- Persisting high psychological risk for 38.5% of parents, which is associated with substantial emotional distress7
- Psychological, physical, and social impacts after their child’s hospitalisation, sometimes for years after discharge8,9
The Findings
Systematic reviews and studies in the field have reported:
- Parent peer support is desirable10
- Psychological support not only needs to be available but also needs to be integrated early6
- Parents would like all family members to have access to counselling6
- Strategies to support the psychological care of parents need to be identified, developed and implemented11
- There is a need for new models of care that address the social, emotional and physical health impacts on parents5
The Model
The goal is to adapt the Maggie’s concept to create a unique built environment within which parents and caregivers who are supporting children and young people through serious illness, such as those with heart problems, cancer, diabetes and cystic fibrosis, can recharge in a quite, supportive space and leave with greater strength and knowledge to not only care for themselves but to support their unwell child and strengthen the bonds within their families.
Young Maggie’s will be a welcoming, homely space, which will put visitors at ease.
It will be a quiet place of nurturance providing parents with:
- an informal, warm environment
- a place to stop
- time out to recharge
- time to unwind
- the opportunity to connect with other parents
- peer support
- free psychosocial support
- access to information
The kitchen table will be the heart of the Centre, where parents can sit, have coffee and cake, meeting other parents and simply take some time. Parents will be able to stay as long as they like and no need to check in or out. The Centre will also have quiet spaces for visitors to have down time, away from others.
The Benefits
By holding and supporting the parent, we can help parents hold and support their child. Following the principles of attachment theory, mindfulness and problem solving therapy, we can help reduce the fear, isolation, stress, anxiety and depression experienced by many parents.
Improved psychological wellbeing
- Sharing experiences with others in a similar situation is associated with a decrease in parent distress and improves parent and child of mental health12
- Specific psychological interventions have improved parents mental health13
A Safe Haven
The aim is to create a safe holding environment for parents, which provides:
- A place of acceptance
- A place for safe self-expression
- A place of resonance with others
- A place of connection with nature
- A place of nurturance of the physical body
Evaluation
It is important to provide evidence-based care. For this reason, research will be a key focal point of our work.
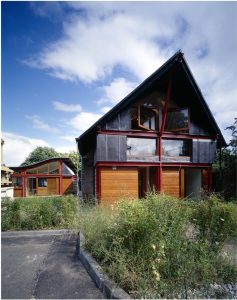
The Build
Maggie Centres
The first Maggie Centre opened in the United Kingdom in1996 and was the idea of cancer patient Maggie Keswick Jencks. Today there are 27 Maggie Centres operating in the UK, a further 6 currently being built and two in Asia (Japan and Hong Kong).
- Maggie centres are designed – pro bono – by leading architects.
- Each Centre is located within close proximity to a hospital where patients receive care and surrounded by nature.
- Centres are designed to be uplifting places to visit – full of light and open space.
- The “kitchen table” is a key aspect of the design, providing a place to sit with others who are in a similar situation, talking and sharing over a coffee.
- Centres provide free practical, emotional and social support
Young Maggie’s
The design and principles will follow Maggie’s. Once a location and funding is found, we aim to:
- Secure pro-bono support for the design
- Be located in close proximity to the Royal Children’s Hospital, Melbourne
- Create an uplifting space – surrounded by nature
- Place the kitchen table at the heart of the Centre
- Provide free practical, emotional and social support
The Team
Executive Team
Dr Catherine Olsson (PhD) is a health psychologist with over 25 years experience working in the loss and grief field. She is s the Founder of Young Maggie’s and leading the translation of findings from the Australian Temperament Project to enhance clinical services to parents caring for seriously ill children.
Dr Katie Moore (MBBS MRCPCH FRACP MBioethics) is a paediatric oncologist & family therapist.
Advisory Board
An Advisory Board has been established and includes 14 eminent clinicians, healthcare related professionals and parents. They play a key role in supporting the Centre to deliver Young Maggie’s programme in a coherent and consistent manner. It will also evaluate the delivery and development of the programme and advises on the implementation of recommendations from programme reviews and audits, ensuring that the programme is effective and of a high quality.
Contact us
We can be contacted via our Facebook page or by email at catherine.olsson@outlook.com
References
- Brehaut JC, Kohen DE, Garner RE, et al. Health among caregivers of children with health problems: findings from a Canadian population-based study. Am J Public Health 2009; 99(7): 1254–1262.
- Remedios C, Willenberg L, Zordan R, et al. A pre-test and post-test study of the physical and psychological effects of out-of-home respite care on caregivers of children with life-threatening conditions. Palliative Medicine 2015; 29(3): 223–230.
- Li J, Precht DH, Mortensen PB, et al. Mortality in parents after death of a child in Denmark: a nationwide follow-up study. Lancet 2003; 361(9355): 363–367
- Muscara F, McCarthy M, Woolf C, Hearps S, Burke K, Anderson V (2015). Early psychological reactions in parents of children with a life threatening illness within a pediatric hospital setting. European Psychiatry 2015; 30: 555-561.
- Collins A, Hennessy-Anderson N, Hosking, Hynson J, Remedios C, Thomas (2016). Lived experiences of parents caring for a child with a life-limiting condition in Australia: A qualitative study. Palliative Medicine, 30(10): 950-959.
- Gill F, Hashem Z, Stegmann R, Aoun S. (2021). The support needs of parent caregivers of children with a life-limiting illness and approaches used to meet their needs: A scoping review. Palliative Medicine, 35(1) 76–96. https://doi.org/10.1177/0269216320967593
- Hearps J, McCarthy M, Muscara F et al (2014). Psychosocial risk in families of infants undergoing surgery for a serious congenital heart disease. Cardiology in the Young, 24, 632-639. https://doi.org/10.1017/S1047951113000760
- Abela K, Wardell D, Rozmus C, LoBiondo-Wood G. (2020). Impact of Pediatric Critical Illness and Injury on Families: An Updated Systematic Review. Journal of Pediatric Nursing 51,21–31. https://doi.org/10.1016/j.pedn.2019.10.013
- Woolf‐King SE, Anger A, Arnold EA, Weiss SJ, Teitel D. (2017). Mental health among parents of children with critical congenital heart defects: a systematic review. Journal of the American Heart Association, 6(2), e004862. https://doi.org/10.1161/JAHA.116.004862
- Heath J., Williamson, H., Williams, L., & Harcourt, D. (2018). Parent perceived isolation and barriers to psychosocial support: A qualitative study to investigate how peer support might help parents of burn-injured children. Scars Burn Heal, 4, 1–12. https://doi.org/10.1177/2059513118763801
- Biber S, Andonian C, Beckmann J, Ewert P, Freilinger S et al (2019). Current research status on the psychological situation of parents of children with congenital heart disease. Cardiovascular Diagnosis and Thearapy, 9(2), S369-S376 http://dx.doi.org/10.21037/cdt.2019.07.07
- Douma M, Bouman C, van Oers H, Maurice-Stam H, Havermann L, Grootenhuis M and Scholten L. (2020). Matching psychosocial support needs of parents of a child with a chronic illness to a feasible intervention. Maternal and Child Health, 24, 1238-1247. https://doi.org/10.1007/s10995-020-02925-3
-
LawE, FisherE, EcclestonC, PalermoTM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No.: CD009660. https://doi.org/10.1002/14651858.CD009660.pub4